What is Multiple System Atrophy?
Multiple System Atrophy (MSA) is a rare disorder that affects the functioning of multiple systems in the brain. Some of these are involved in the control of movement, balance and coordination, while others ensure blood pressure, bladder, bowel and sexual function.
Patients may experience:
- Slowness of movement, muscle stiffness and/or shaking/tremor
- Problems with balance and coordination
- Feeling lightheaded or dizzy while standing
- Problems controlling bladder function and constipation
MSA is one type of Atypical Parkinsonism. Atypical Parkinsonism, also called Parkinson-plus syndrome, is when the patient has some of the main features of Parkinson’s disease (PD) such as slowness of movement, muscle stiffness and/or shaking/ tremor, as well as some other features. Patients with slowness, muscle stiffness or shaking may resemble patients with PD and are called MSA-P. Patients who have more difficulty with balance and coordination are called MSA-C.
These disorders were formerly known as:
- MSA: Shy-Drager syndrome
- MSA-P: striatonigral degeneration (SND)
- MSA-C: sporadic olivopontocerebellar atrophy (OPCA)
Who gets MSA?
MSA affects men and women equally. MSA usually begins between the age of 50 and 60. MSA is considered rare and affects around three to four people in every 100,000.
What Is the Cause?
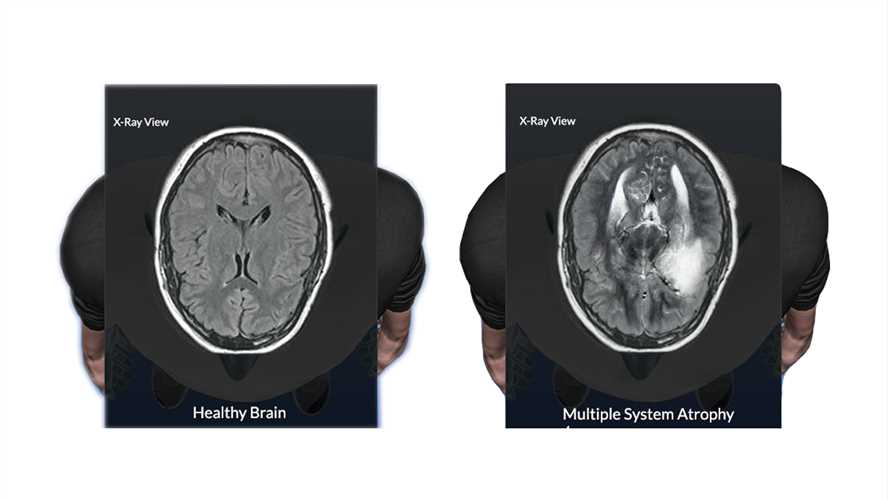
The cause is unknown. MSA is associated with accumulation of a protein in the brain called alpha-synuclein that clumps up in different cell types and can be seen in a brain autopsy. The cause of this clumping is unknown. MSA has been described in a few families, but is currently not considered a hereditary disease. MSA is not contagious or spread from person to person.
How is MSA diagnosed?
A diagnosis may not be clear at first. MSA is usually diagnosed based on symptoms and physical examination findings. Tests may include brain MRI scan, bladder tests, and testing for blood pressure changes, including the table tilt-test.
Is there a treatment?
There are currently no treatments to cure, slow down or reverse MSA. However, some medications and physical therapies may help your symptoms.
Parkinson-like symptoms of slowness, stiffness, and tremor may improve with medications typically used for PD.
Low blood pressure when moving into a sitting or standing position (orthostatic hypotension) may improve by avoiding triggers like alcohol, dehydration, and heat or hot temperatures. You may need to adjust or stop medications for other illnesses, especially those that might lower blood pressure. Doctors may advise increasing water and salt intake or using abdominal bandages or pressure stockings. In addition, specific medications may help increase blood pressure. Stable blood pressure helps you avoid unsteadiness, lightheadedness, and dizziness that contribute to falling or balance problems.
For bladder and bowel problems, options include medications, regular toileting, bladder training, and catheterization.
Drooling can be treated with medications and botulinum toxin injections into the saliva glands.
Overall health may also benefit from physical therapy, occupational therapy, or speech and swallowing therapy.
What can I expect as I live with MSA?
Over time, symptoms increase and treatments become less effective. You may experience difficulties using utensils, swallowing solid food or liquids, walking and controlling bladder
or bowels. In advanced stages, MSA patients have increased risk of infections. Bladder symptoms can lead to urinary tract infections. Swallowing problems increase the risk of pneumonia. Overall, long-term care planning may be needed as the disease progresses.